We all have medical questions that we want answered – that’s why Dr. Amna Asif is here to provide us with her expert opinion! Every other week, she will be sharing her expert advice with us regarding a range of topics our followers are interested in learning more about. This week in Doc Talk, she talks about irritable bowel syndrome, more commonly referred to as IBS. Read ahead to find out what exactly it is, what the causes and symptoms are, and what you can do to maange it:

What Is IBS?
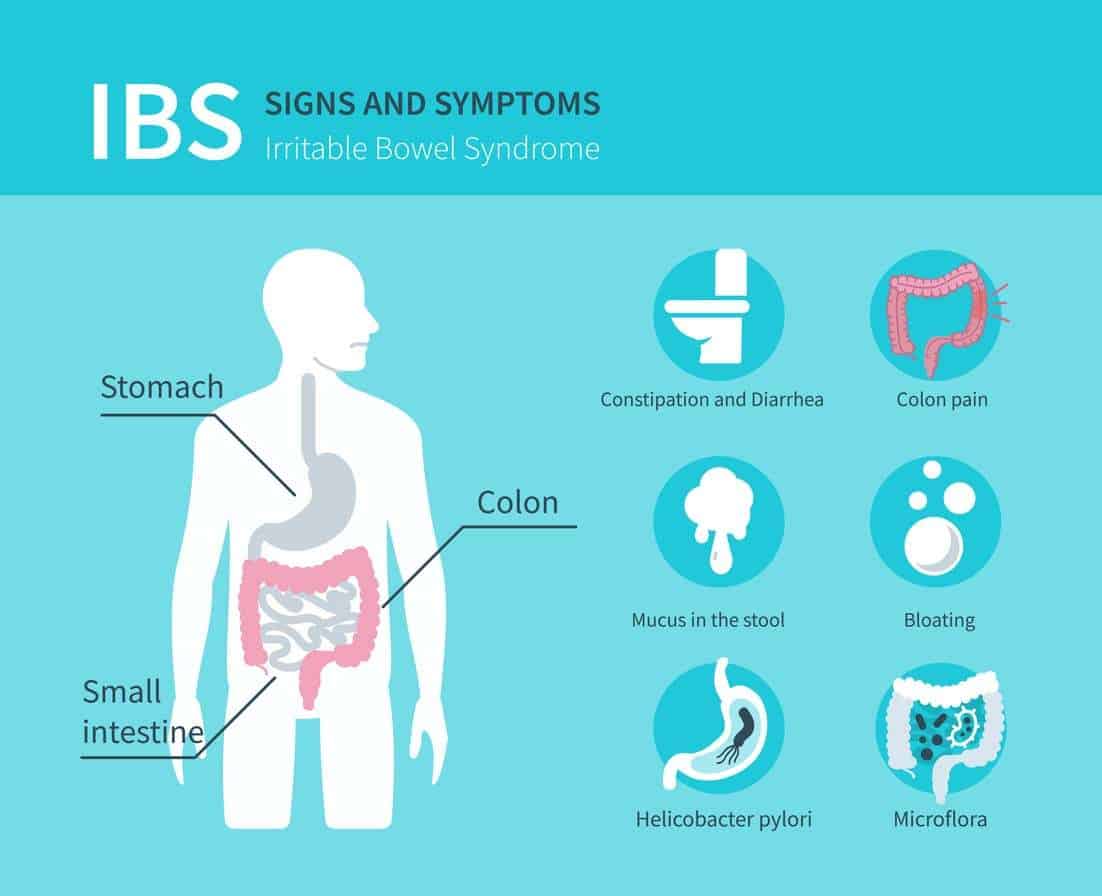
Irritable bowel syndrome (IBS) is a condition that affects the colon (large bowel). Although it is not considered life-threatening or dangerous, it can be very uncomfortable. It is common and affects around 3 out of every 10 people. Women are more likely to be affected than men and the symptoms usually start in early adulthood.
IBS is different from inflammatory bowel disease (IBD) and is a functional disorder. The cause is unknown, but environmental factors such as changes of routine, emotional stress, infection and diet can trigger an attack. Research has shown that the neurotransmitter serotonin may be important in the symptoms of IBS, by altering the function of nerve cells in the bowel and causing changes in pain sensation and bowel function.
Irritable bowel syndrome doesn’t cause lasting damage and doesn’t contribute to the development of serious bowel conditions, such as cancer or colitis.
Causes
The underlying cause is still unknown, but certain factors have been found to ‘trigger’ attacks in susceptible individuals. These include:
- Infection – an episode of gastroenteritis will often result in persistent bowel symptoms, long after the offending bacterial or viral infection has resolved. Up to 25% of IBS may be due to this problem.
- Food intolerance – impaired absorption of the sugar lactose (found in dairy and many processed foods) is the most common dietary trigger for IBS. Other sugars believed to trigger IBS are fructose (present in many syrups) and sorbitol.
- General diet – low-fibre diets can exacerbate the constipation of constipation predominant IBS. Some people find spicy or sugary foods cause problems. However, many experts are sceptical about the role of general diet itself.
- Emotional stress – strong emotions, such as anxiety or stress, can affect the nerves of the bowel in susceptible people.
- Medication – certain types (such as antibiotics, antacids and painkillers) can lead to constipation or diarrhoea.
Symptoms
These may include:
- Abdominal pain or cramping that is often relieved by passing wind or opening bowels
- Alternating diarrhoea and constipation
- A sensation that the bowels are not fully emptied after passing a motion
- Abdominal bloating
- Mucus in the stools
- Nausea.
None of these symptoms are exclusive to IBS. It is unusual for IBS to produce these symptoms for the first time, after the age of 40.

Main IBS Categories
Irritable bowel syndrome can be subdivided into three major categories:
- Constipation-predominant – the person tends to alternate constipation with normal stools. Symptoms of abdominal cramping or aching are commonly triggered by eating.
- Diarrhoea-predominant – the person tends to experience diarrhoea first thing in the morning or after eating. The need to go to the toilet is typically urgent and cannot be delayed. Incontinence may be a problem.
- Alternating constipation & diarrhoea.
Diagnosis Of IBS
If you suspect you have IBS, it is important to seek medical advice to make sure your symptoms aren’t caused by any other illness, such as diverticulitis, inflammatory bowel disease or polyps. Coeliac disease (an immune intolerance to gluten, present in wheat and other grains) may produce many of the same symptoms as IBS. Lactose intolerance may produce bloating, cramps and diarrhoea.
The investigations include:
- full medical check-up
- blood tests, including blood tests for coeliac disease
- stool tests
- investigation of the bowel under sedation (colonoscopy) or barium enema, if necessary.
Treatment
IBS cannot be cured with medication or special diets. The primary preventative measure is to identify and avoid individual triggers. Treatment options may include:
- A modest increase in dietary fibre, along with plenty of clear fluids.
- Reducing or eliminating common gas-producing foods, such as beans and cabbage.
- Reducing dairy foods, if lactose intolerance is a trigger.
- Antidiarrheal medication – these can be an essential part of management in those with diarrhoea-predominant IBS.
- Pain-relieving medication – opiates such as codeine can provide effective pain relief.
- Medications to treat constipation.
- Antispasmodic drugs, which may ease cramping – examples include mebeverine, belladonna, hyoscine and peppermint oil capsules.
- Tricyclic antidepressants – these can be effective in treating the pain of IBS. Use of these does not mean that IBS is caused by depression.
- Stress management, if stress seems to be triggering the attacks.
- Establishing eating routines and avoiding sudden changes of routine.
A group of carbohydrates called FODMAP is now believed to contribute strongly to symptoms of IBS in many people. A low-FODMAP diet can be tried in these instances. This diet can be commenced with the supervision of a dietician experienced in management of IBS.
People with IBS can become frustrated and feel their symptoms are not treated seriously. These frustrations, along with sometimes inappropriate therapy, can often make the symptoms worse. Finding a therapist (Doctor & dietician) with experience in successful treatment of IBS is important.







What do you think?
You must be logged in to post a comment.