Post-coital bleeding is the term used for vaginal spotting or bleeding that occurs after sexual intercourse and is not connected to the regular menstrual cycle. While this type of bleeding is often painless, it can sometimes be accompanied by dyspareunia or pain during intercourse. Understanding the underlying causes of post-coital bleeding is crucial for identifying effective treatment options and addressing any potential health concerns. In this article, we’ll explore the main causes and what steps can be taken to seek appropriate care.

Common Causes of Post-Coital Bleeding
1. Cervicitis:
Cervicitis is the inflammation of the lower part of the cervix that can be accompanied by watery or mucopurulent vaginal discharge. Inflammation makes the cervical lining fragile, which can lead to spotting after intercourse. Acute cervicitis is typically caused by bacterial infections and can be conveniently treated with appropriate antibiotic medication. Chronic cervicitis generally does not have an infectious source. Early diagnosis of cervicitis and timely treatment can help prevent complicated scenarios, such as chronic pelvic pain and pelvic inflammatory disease.
2. Endometrial Infections:
Acute or chronic infections of the internal lining of the uterus can also cause post-coital bleeding. Treatment for this condition requires appropriate antibiotics.
3. Cervical Polyps:
Cervical polyps are non-cancerous small growths that protrude from the cervical canal. These often need to be surgically removed, as they can become irritated and bleed after intercourse.
Cervical Cancer and Screening
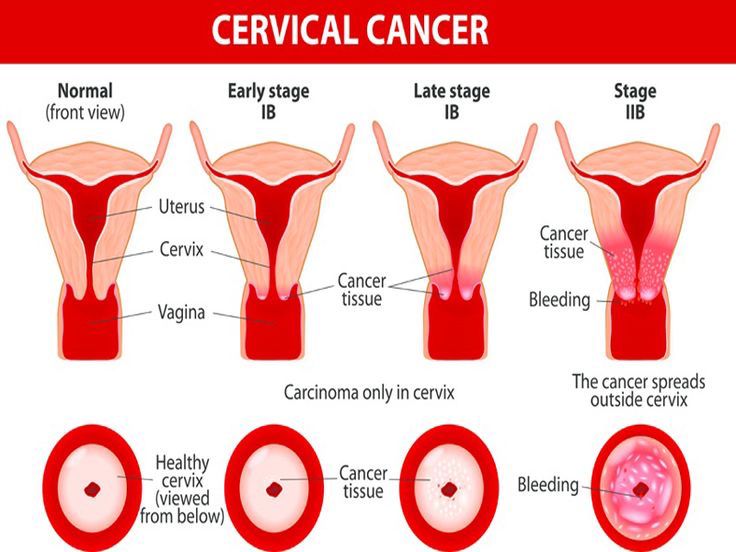
Cervical Cancer:
Cervical cancer is the second most common cancer in women worldwide. Risk factors include human papillomavirus (HPV), immunosuppression, and smoking. According to the American College of Obstetricians and Gynecologists (ACOG), women should have regular cervical cancer screenings. Screening should start at age 21; from ages 21 to 29, pap smears should be conducted every three years. For women aged 25 to 29, HPV testing can be done alone, but pap tests are preferred.
For women aged 30 to 65, there are three options: they can have a pap test and HPV co-tests every five years, a pap test alone every three years, or HPV testing alone every five years. The pap test is a procedure in which a small brush is used to collect cells from the surface of the cervix so they can be studied under a microscope. Your gynecologist can recommend the screening protocol that is appropriate for you. Cervical cancer screening can detect abnormal changes long before they develop into cancer.
HPV Vaccine:
The HPV vaccine, Gardasil 9, was approved by the U.S. FDA (Food and Drug Administration) in 2014. It can be administered to individuals aged 9 and older. The CDC (Centers for Disease Control and Prevention) recommends routine HPV vaccination at ages 11 or 12. Gardasil protects against genital warts and most cases of cervical cancer, as well as cancers of the vagina and vulva. The FDA approved the use of Gardasil 9 for males and females aged 9 to 45 years. The HPV vaccine is not recommended during pregnancy, after experiencing allergic reactions following the first HPV shot, or in cases of severe life-threatening allergies. You can consult your physician to learn more about the Gardasil 9 vaccine and discuss how you can benefit from it.
Other Causes of Post-Coital Bleeding
Other causes of post-coital bleeding include hormonal birth control pills that can change bleeding patterns in some women, incorrectly positioned intrauterine devices (IUDs), and trauma from injury during intercourse. In some cases, no clear cause is identified.
.





What do you think?
You must be logged in to post a comment.